A major obstacle in clinical practice and research is hyperprolactinemia, a disorder marked by increased blood levels of the hormone prolactin. This article explores the most recent developments and breakthroughs in the study of hyperprolactinemia, from cutting-edge pharmacological therapies to innovative diagnostic techniques. This thorough study attempts to shed light on the changing landscape of comprehending and treating this complicated endocrine illness by examining the present difficulties in managing hyperprolactinemia and the possible treatment targets of the future.
Hyperprolactinemia is a medical disease that requires awareness and is not simply a mouthful. To put it simply, hyperprolactinemia is the excessive amount of the prolactin hormone in the blood. Furthermore, it won't suddenly cause you to start making milk.
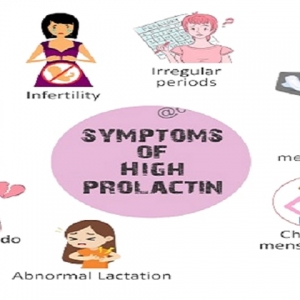
Think of prolactin as your body's method of controlling reproductive function, somewhat like that buddy who is always arranging things. Overproduction of prolactin may cause a number of problems, including irregular menstruation, infertility, and unexpected milk production (yes, even in men).
Finding a unicorn may not be as uncommon as hyperprolactinemia, since research indicates that 1 in 5 women of reproductive age may be affected. Pituitary gland compression symptoms may be as minor as headaches and visual issues, or as noticeable as changes in menstrual cycles and breast milk supply.
Cabergoline Treat high concentration of the hormone prolactin in the blood is known as hyperprolactinemia. During breastfeeding, the pituitary gland releases the hormone prolactin, which primarily boosts milk production. Among the many health issues that may arise from an abnormal rise in prolactin levels are menstrual cycle abnormalities, infertility, and erectile dysfunction. Cabergoline eliminates these issues by regulating prolactin levels.
Consider the study of hyperprolactinemia as attempting to solve a hormonal enigma. The more we comprehend about this illness, the more prepared we are to create specialized remedies and raise the standard of living for individuals impacted. Not only is science important, but also really impacting people's lives.
There are challenges unique to managing hyperprolactinemia, such as avoiding side effects from conventional medications and adjusting to the impact on daily living.
Conventional therapies for hyperprolactinemia often include drug regimens that may have a range of negative effects, from nausea and vertigo to more severe problems including loss of bone density. It's similar to attempting to solve one issue while unintentionally creating many others.
controlling the emotional toll that hyperprolactinemia may have is just as important as controlling the physical symptoms. Imagine attempting to manage your relationships, career, and self-care while dealing with infertility or persistent exhaustion. It's an acrobatic performance that nobody choose.
Recent developments in imaging technology and biomarkers are transforming the landscape of hyperprolactinemia diagnosis.
Forget blurry pictures; MRIs and other contemporary imaging modalities provide a more precise view of the pituitary gland and enable medical professionals to identify any anomalies that may be contributing to the overproduction of prolactin. Comparable to switching from a flip phone to a smartphone, it offers improved clarity and decision-making.
Effective treatment of hyperprolactinemia depends on early identification. Biomarkers, which may be thought of as microscopic indicators found in saliva or blood, are being researched to identify hormonal imbalances before they cause major problems for your health. It's similar to being aware of impending storms.
With the development of novel medication classes and customized medicine strategies, the treatment of hyperprolactinemia seems to have a bright future.
Bid adieu to the strategy that satisfies all needs. Specialized medication classes with distinct mechanisms of action are being developed to precisely treat hyperprolactinemia. Precision is important, just as when you upgrade from a general-purpose tool to a specialist instrument.
Since every body is unique, why should medical interventions be too? When it comes to hyperprolactinemia, personalized medicine entails adjusting treatment plans depending on a patient's unique genetic makeup and hormone levels. You deserve nothing less than a treatment plan that is specifically tailored to your body's requirements.
In an effort to understand how certain genes affect the development of hyperprolactinemia, researchers are exploring the genetic foundations of the condition. A better understanding of the complex processes behind this illness may be gained by examining how hormones such as estrogen and dopamine influence prolactin levels.
Cabergoline 0.5mg Tablet is a dopamine agonist. It is used to treat elevated levels of prolactin. It may also assist halt breast milk production in situations of stillbirth, abortion, or miscarriage. Cabergoline 0.5 Tablet should be taken with meals, but only at the same time for the best results. It should be interpreted as your physician's advice.
Investigating the function of neurotransmitters like serotonin and dopamine in prolactin production provides fresh perspectives on the intricate interactions between the brain and the endocrine system in hyperprolactinemia.
By examining novel molecular pathways, tailored medicines that have the potential to transform the treatment of hyperprolactinemia may be developed. Researchers hope to lessen adverse effects and increase therapeutic success by identifying new targets.
The use of gene therapy and immunotherapy in the treatment of hyperprolactinemia offers hope for targeted and individualized approaches. Novel approaches to addressing this endocrine condition include altering hereditary variables and leveraging the body's immunological response.
By combining artificial intelligence and big data analytics, researchers may now analyze enormous volumes of data and get important insights for their studies on hyperprolactinemia. By using these technologies, the illness is better understood and customized treatment plans are developed more quickly.
Thanks to telemedicine, patients with hyperprolactinemia may get better treatment since consultations, monitoring, and assistance can be provided remotely. Its integration improves patient outcomes and management efficiency by making specialist healthcare services more accessible.
To sum up, the continuous progress in the study of hyperprolactinemia has the potential to enhance patient outcomes, therapeutic effectiveness, and diagnostic precision. The treatment of hyperprolactinemia looks to have a more promising future with the incorporation of technology breakthroughs and a clearer knowledge of the pathophysiology. It's clear that tremendous strides are being made in improving the treatment and wellness of people with hyperprolactinemia as long as researchers keep pushing the envelope of knowledge and creativity in this area.